New Therapy May Aid Heart Repair After Heart Attack
Researchers Quantify Improvement in Heart Vasculature with Vesselucida 360 and Vesselucida Explorer
Cells need oxygen to survive, but during a heart attack, blood flow is restricted and cardiac cells can’t get the oxygen they need to stay alive. A new therapy, developed by researchers at the Coulombe Lab at Brown University may be able to provide the heart with the support it needs to recover after a heart attack, according to a study published in the journal Biomaterials.
Using Vesselucida 360 and Vesselucida Explorer to quantify blood vessels in the rat heart, the research team, led by Dr. Fabiola Munarin, observed improved cardiac function and saw evidence of revascularization 30 days after implanting engineered tissue into injured rat hearts. Critical elements in the implanted tissue included heart muscle cells derived from human pluripotent stem cells and alginate microspheres loaded with angiogenic growth factors (VEGF, bFGF, and Sonic Hedgehog).
By embedding this combination of heart cells and loaded alginate microspheres into the implanted tissue, the scientists were able to support the heart’s vascular network by delivering growth factors to the injured muscle. These growth factors worked with host cells to stimulate regeneration in the injured heart.
After implanting the engineered tissue, the researchers monitored the rats’ heart function over the next four weeks. They observed improvements in rats that had received tissue containing alginate microspheres loaded with angiogenic growth factors versus control groups, which had received either sham implants, only heart cells, or heart cells and unloaded alginate microspheres.
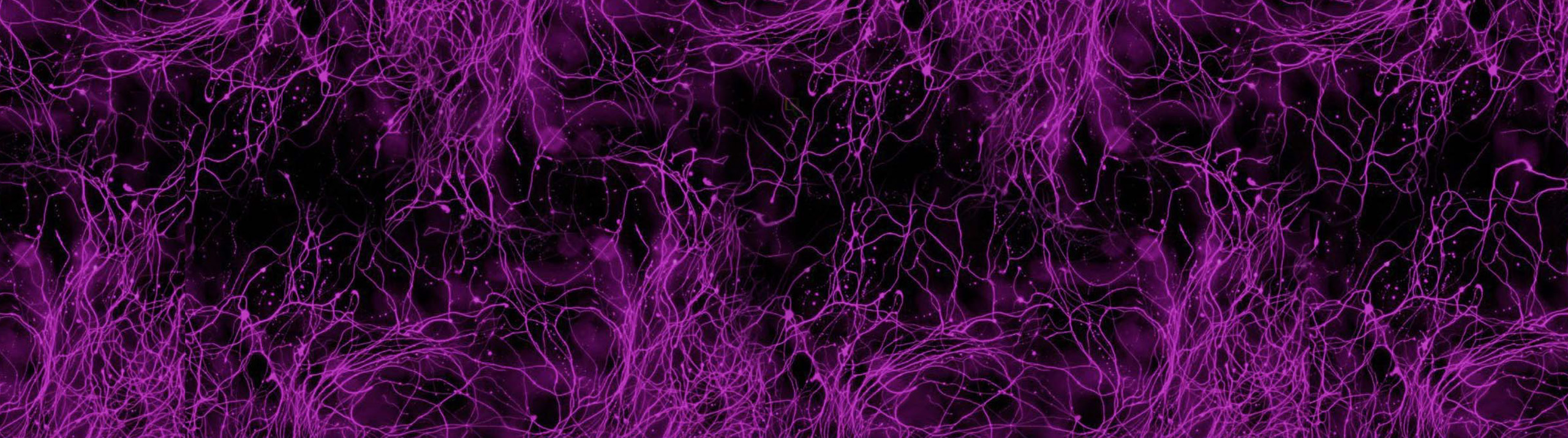
Thirty days after implantation, the research team sectioned 23 hearts. They made 3D reconstructions of four of them, after clearing and imaging with a florescence microscope. They then turned to Vesselucida 360 and Vesselucida Explorer to quantify vascular growth.
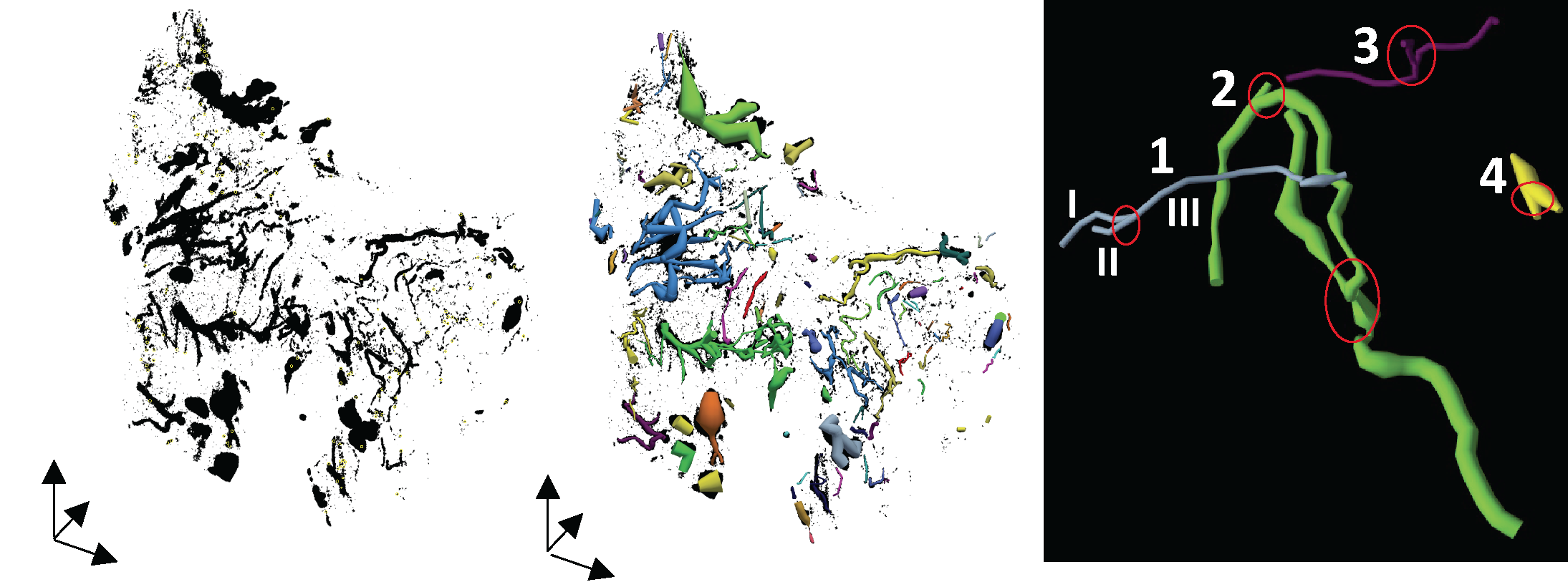
Image source: https://doi.org/10.1016/j.biomaterials.2020.120033
“After examining different vessel quantification tools for use with neovessel formation in the heart, we chose to use Vesselucida 360 because it offered us flexibility in viewing and adjusting vessel geometries in 3D to accurately represent our microCT dataset. Also, the quantitative parameter extrapolation is excellent,” explained Dr. Kareen Coulombe.
Tracing the blood vessels in the four 3D heart reconstructions with Vesselucida 360, and then using Vesselucida Explorer for automated analysis, revealed an increase in vascular network density, vessel length, branching, and a wider distribution of blood vessel diameters. They also observed reduced tortuosity, or distortion of the vessel pathways — a sign that blood could travel more freely to the heart.
“Our results show for the first time the beneficial effects of integrating cardiac engineered tissues with a localized angiogenic therapy. With this combined therapy, we are able to induce the formation of new functional and perfused vessels in the implanted cardiac tissue, the revascularization of the ischemic heart, and the improvement of whole heart function.” (Munarin, et al 2020)
Munarin F, Kant RJ, Rupert CE, Khoo A, Coulombe KLK, Engineered human myocardium with local release of angiogenic proteins improves vascularization and cardiac function in injured rat hearts, Biomaterials (2020), doi: https://doi.org/10.1016/j.biomaterials.2020.120033.


